Dr. Hongyun Huang transplants OEG cells obtained from the brains of aborted fetuses into patients at Xishan Hospital near Beijng, China. While the OEG cells Dr. Hwang uses are not obtained from the patient, he reports that there have not been problems with rejection. To qualify for surgery the patient cannot have a complete transection (separation) of the spinal cord (a rare occurrence). Dr. Huang has performed the procedure on hundreds of patients and claims there has been some improvement in 70% of the individuals operated on. The length of time from the date of spinal cord injury to surgery has ranged from six months to 18 years. Treatment cost is about $20,000 (excluding travel costs and lodging) and the average stay in China is about one month. There have been some complaints from patients who have traveled to China about the quality of Chinese hospitals. Dr. Huang originally operated at Chaoyang Hospital but has since moved to Xishan Hospital, apparently at least in part due to complaints about the quality of Chaoyang Hospital. .
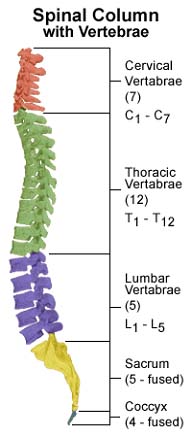
A different approach to the use of olfactory cells has been taken by a team headed by Drs. Tim Gerahty and Alan McKay-Sims at Princess Alexandria Hospital in Brisbane, Australia. They remove olfactory tissue from the patient and then culture it to grow additional cells. The cells (around 12,000,000) are then injected into the area of the injury. The injections do not require surgery. Some researchers question whether cells injected into the spinal cord will remain in the area of injury, given that cerebrospinal fluid bathes the cord and can wash the cells to other parts of the central nervous system, including the brain. The Brisbane team limited the patients in their small study (8 patients) to individuals with complete spinal cord injuries in the thoracic area that are six months to three years old. Results of their study, which began in 2001 and was scheduled to end in 2004, have not been published.
Another source of stem cells is the blood. Most blood cells (red and white) are made from a high concentration of stem cells in the bone marrow. However, there are some stem cells in the blood itself. While adults do not have enough stem cells in their blood to make it worthwhile to collect them, newborn babies have a much higher concentration of stem cells in their blood. After babies are delivered a small amount of their blood (3 – 5 ounces on average) remains in the umbilical cord. At one time the umbilical cord and any blood it contained were simply discarded. However, some blood banks have begun to collect and store umbilical cord blood.
The stem cells from “cord” blood have been used to treat people with some blood disorders, such as leukemia. Leukemia is a type of cancer involving white blood cells. To treat leukemia it is often necessary to administer high doses of chemotherapy that kill all of the stem cells in the patient’s bone marrow, where the cancer cells are produced. Because white and red blood cells are necessary for life, the dead stem cells must be replaced with cells from a donor. However, the donor’s cells must “match” the type of the patient to prevent rejection by the immune system. Replacement stem cells have usually come from bone marrow donors. The stem cells are isolated from the marrow and then injected into the patient’s blood. When the procedure is successful, the donated stem cells migrate to the bone marrow (because this is what stem cells ordinarily do) and then begin producing normal red and white blood cells .
However, stem cells from cord blood can be used in place of a bone marrow transplant and have a number of advantages. First, it can be difficult to find a bone marrow donor with a type that matches the patient’s. Because cord blood can be banked for years, there are many donors, and it is already “typed,” a suitable match can more easily and quickly be found. Second, cord blood is a safe, relatively inexpensive, and readily available source of stem cells. Bone marrow donations, on the other hand, require that the donors undergo a surgical procedure. The surgery is financially costly and exposes the donor to the potential risks and complications of any surgical procedure. Third, the genetic markers on a baby’s stem cells are not as prominent as those in adults, reducing the risk of rejection that exists even with a matched donor.
Cord blood stem cells are now being investigated in spinal cord transplantation. Professor Song Chang-hun and others at Chosun University in South Korea have injected cord blood stem cells into patients’ spinal cords. One patient who had been unable to walk for twenty years reportedly was able to walk with a walking frame after the injection. However, this outcome has not been duplicated in other patients or by other researchers. Injections of cord blood stem cells are being performed at Nan Shan Hospital in Shen Zhen, China, just across the border from Hong Kong. However, the focus at that institution has been on treating brain injuries and other brain disorders. One question among many regarding cord stem cells is whether they will differentiate into neurons when injected into the central nervous system.
There are some physicians in various parts of the world who claim that injecting umbilical cord stem cells into a patient’s blood will cure or improve a host of conditions, ranging from diabetes to multiple sclerosis to spinal cord injuries. There is no reliable evidence to support these claims. Stem cells in the blood have a limited lifetime and will ordinarily gravitate into the bone marrow. There is no evidence to suggest that stem cells will somehow selectively travel in the blood to an area of injury or disease, manage to pass out of a blood vessel at that location and into the injured tissue, and then transform themselves into the type of tissue that is injured. Furthermore, even if some stem cells managed these feats, others might not differentiate and instead form a tumor. The physicians performing these “treatments” typically charge large sums and have never subjected their results to the scrutiny of the scientific and medical communities.
In the United States new medical treatments must be approved by the Food and Drug Administration. Before the FDA will approve a proposed treatment, it must go through several stages of testing, beginning in a test tube, followed by laboratory animals and then progressing to carefully controlled experimental trials with people. The FDA has not yet approved stem cell transplantation for even experimental trials with people.
People with serious spinal cord injuries are understandably anxious and eager to find some treatment that will improve their condition. Does stem cell transplantation currently offer a realistic hope of improving the functional or pain levels of spinal cord injury survivors? The methods and results of the handful of surgeons in the world currently transplanting tissue into injured spinal cords have not been the subject of the kind of careful reporting and scrutiny by the medical and scientific communities that need to occur before reliable conclusions can be drawn. What is known is that a great deal remains to be learned about repairing an injured spinal cord. As with any surgery, transplantation surgery has potentially serious risks and complications. Furthermore, because surgery always creates scarring, it may be more difficult to perform surgery in the future – when the chances of a successful outcome are likely to be greater than they are today – in cases where a survivor has already undergone an unsuccessful transplant surgery. The survivors who describe some improvement following transplant surgery generally report that it is not dramatic and requires a dedicated commitment to rehabilitation. Some survivors have also reported that improvement following surgery was not permanent.
See also: Cell Transplantation for Spinal Cord Injury: A Systematic Review