The primary assessment of a patient with trauma in the field follows the ABCD prioritization scheme:
Any patient that has sustained a head injury and appears confused or is unconscious should be considered to have a traumatic spinal injury. If the patient is alert and indicates they have spinal pain, numbness or weakness the first responders also make the cautious assumption of an SCI. Any presumed spinal injury should be handled with extreme care and the patient should be immobilized.
Using a log-roll technique, the paramedics or other responders place the patient onto a backboard for transfer and ft the patient with a rigid cervical collar.
Hospital emergency departments follow the same ABCD scheme when evaluating SCI patients. Injuries that are life-threatening - e.g. breathing difficulties, systematic bleeding, a pneumothorax - take priority over the presumed spinal injury.
There are several types of treatment in the short term for a spinal cord injury. First, the spine in the area of the injured spinal cord is immobilized (held in place so it can’t move) to prevent further injury to the cord. For injuries to the neck, immobilizing the spine may include placing the head in a “halo” (a device that prevents the head from moving). For spinal cord injuries in the back, casts, braces and straps may be temporarily used to keep the back from moving.
To reduce swelling in the spinal cord caused by injury, steroid medication is usually given during the first 24 hours following injury. Other medical treatment is often necessary, depending on complications that may develop.
Because traumatic injury to the spinal cord usually involves an injury to the bones and ligaments of the spine, surgery may be performed. The aim of some surgeries is to remove bone (this is called "decompression") that is pressing on or into the spinal cord. A surgeon may also want to stabilize or realign the spine in the area of the spinal cord injury when the vertebrae or ligaments have been damaged. Metal rods or cages and screws may be attached to normal vertebrae to prevent movement of fractured vertebrae and the vertebrae may be “fused” together using bone graft for the same reason. Grafts, which involve the growth of new bone tissue into adjacent bone, require time to “take”. Consequently, metal “hardware” is usually needed to hold the spine in place while the graft is taking. Stretching of the spine using weights and pulleys (called traction) may also help with alignment of the spine.
Rehabilitation hospitals provide several different types of specialists to help in the recovery process. Physicians who specialize in physical and rehabilitation medicine (called physiatrists) usually supervise the rehabilitation program. Physical therapists plan therapy to strengthen muscles in parts of the body that still function. Occupational therapists specialize in training individuals who have lost muscle strength or coordination to relearn the tasks of daily living, such as eating, dressing, and grooming. They also train people in how to use assistive equipment and braces. Social workers help in finding resources to pay for equipment, home modifications, and attendant care. Family members also receive education in assisting the injured person.
Some news about stem cell research into spinal cord injury treatment. And stem cell research into SCI treatment
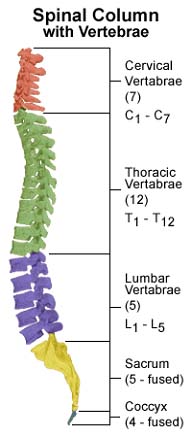
Whether a spinal cord injury is permanent or not will depend in part on how severe the injury is, which can range from a mild bruise (contusion) to the cord being severed in two. Even when injuries are permanent, any survivors, including those with severe spinal cord injuries, achieve a one or two level of “functional” improvement following treatment and rehabilitation (and some survivors achieve an even better recovery). For example, a patient who has a spinal cord injury at the C5 vertebral level might well be functioning at a C6 or C7 level after rehabilitation. While this might not seem important, a one level improvement in the neck may enable a person on a respirator to breathe independently or a person who would otherwise be dependent on others to be independent in the community.This occurs when there has been some regeneration in the spinal cord below the level of the injury. The following chart illustrates the functioning commonly associated with spinal cord injuries at various levels.
| Level | Motor Abilities | Functional Goals for Survivor |
|---|---|---|
| C1-C3 | Limited movement of head and neck |
Breathing: Depends on a ventilator
for breathing. Communication: Talking may be very limited or impossible. If ability to talk is limited, communication can be accomplished independently with a mouth stick and assistive technologies like a computer for speech or typing. Effective communication allows the survivor to direct caregivers with daily activities such as bathing, dressing, personal hygiene, transferring, and bladder and bowel management. Daily tasks: Assistive technology allows for independence in tasks such as turning pages, using a telephone and operating lights and appliances. Mobility: Can operate an electric wheelchair by using a head control, mouth stick, or chin control. A power tilt wheelchair allows independent pressure relief from sitting in one position. |
| C3-C4 | Usually has head and neck control.
Individuals at C4 level may shrug their shoulders. |
Breathing: May initially require a ventilator for
breathing but usually adjusts to breathing full-time without ventilator
assistance. Communication: Normal. Daily tasks: With specialized equipment may have limited independence in feeding and independently operating an adjustable bed with an adaptive controller. |
| C5 | Typically has head and neck control,
can shrug shoulder and has shoulder control. Can bend elbows and
turn palms face up. |
Daily tasks: Independence with eating,
drinking, face washing, brushing teeth, face shaving and hair care
after assistance in setting up specialized equipment. Health care: Can help in preventing pressure ulcers by leaning forward or side-to-side. |
| C6 | Has movement in head, neck, shoulders,
arms and wrists. Can shrug shoulders, bend elbows, turn palms up
and down and extend wrists. |
Daily tasks: With help of specialized
equipment can perform with greater ease and independence daily tasks
of feeding, bathing, grooming, personal hygiene and dressing. May
independently perform light housekeeping duties. Health care: Can independently perform skin checks, turn in bed, and relieve pressure while sitting. Mobility: Some individuals can independently do transfers but often require a sliding board. Can use a manual wheelchair for daily activities but may use power wheelchair for greater independence. |
| C7 | Has similar movement as an individual
with C6 with added ability to straighten elbows. |
Daily tasks: Able to perform household duties.
Needs fewer adaptive aids in independent living. Health care: Able to do wheelchair pushups for pressure relief. Mobility: Daily use of manual wheelchair. Can transfer with greater ease. |
| C8-T1 | Has added strength and coordination
of fingers with limited or even normal hand function. |
Daily tasks: Can live independently
without assistive devices in feeding, bathing, grooming, oral and
facial hygiene, dressing, and bladder and bowel management. Mobility: Uses manual wheelchair. Can transfer independently. |
| T2-T6 | Has normal motor function in head,
neck, shoulders, arms, hands and fingers. Has increased use of rib
and chest muscles and may have some trunk control. |
Daily tasks: Should be totally independent with all
activities. Mobility: A few individuals are capable of limited walking with extensive bracing. However, this requires extremely high energy and puts stress on the upper body, which can lead to damage of upper joints. There is no functional advantage with this kind of walking. |
Because of the force that is required to fracture the spine, many spinal cord-injured patients suffer significant damage to the chest or abdomen. Many of these associated injuries are fatal. For isolated spinal cord injuries the mortality after one year is about 5-7%. If a patient survives the first 24 hours after spinal cord injury, the likelihood of survival for ten years is approximately 75-80%. The ten-year survival rate for patients who survived the first year after injury is 87%. Not surprisingly, younger survivors and those with incomplete injuries do better than older survivors and those with complete injuries.