Osteopenia is a condition where the bone density is lower than normal but not so low that it meets the criteria for osteoporosis. The term is derived from the Greek words osteo, meaning bone and penia, meaning poverty. Literally, osteopenia means "poor bone".
Osteopenia is a loss of mineral density within bone tissue. Sometimes fancifully called osteoporosis light. osteopenia is on the same continuum of bone density with osteoporosis; the two conditions are linked although not everyone with osteopenia will develop osteoporosis. Osteopenia itself is not classified as a disease; it's more properly called a condition.
Most osteopenia cases are caused by the same things that cause osteporosis. Also, people with kidney damage often suffer renal osteodystrophy and that results in osteopenia much of the time.
Like osteoporosis, osteopenia has been described as a "silent" condition. There are no outward signs or symptoms, although certain risk factors can be identified.
| Normal | Bone mineral density (BMD) greater than 1 standard deviation below the mean for young adults |
| Osteopenia | BMD between 1-2.5 standard deviation below the mean for young adults |
| Osteoporosis | BMD more than 2.5 standard deviation below the mean for young adults |
| Severe osteoporosis | BMD more than 2.5 standard deviation below the mean for young adults plus one or more fragility fractures. |
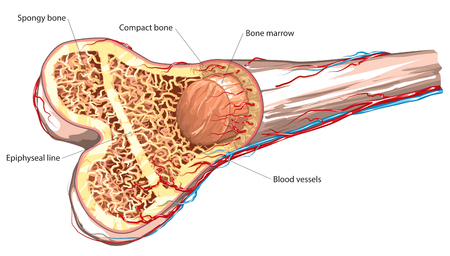
Osteopenia is determined based on the findings of bone mineral density (BMD) testing. A machine called a DXA machine (DXA stands for dual energy x-ray absorptiometry) is used to measure the amount of bone mineral in a certain area. Testing can be performed on your forearm, wrist, hand, hip, spine, or foot. BMD tests are important tools in the arsenal of bone medicine diagnosis, and they are commonly ordered by doctors.
When X-rays of bones with osteopenia show “increased radiolucency” - more x-rays get through the bone than do for healthy bone, but x-rays are not reliable as a way to diagnose thinning bone mass.
The findings of a BMD test are classified according to comparison with average values of healthy subjects which provides a T-score. A T-score, between -1.1 and -2.4 identifies osteopenia. The lower the T-score (higher the negative number), the higher the risk for bone fracture.
When a doctor tells a patient she has osteopenia, there is often some confusion. Osteopenia is NOT osteoporosis, and indeed almost everyone gets osteopenia past a certain age. Even at age 30 a significant fraction of the population has osteopenia – remember, any bone density less than a standard deviation below average counts as osteopenia. Gwyneth Paltrow announced to the world she had osteopenia when she was in her late 30s, but so do millions of other women. A diagnosis of osteopenia per se is not something to worry about, but must be looked at in the context of the patient’s overall health and life.
Most cases of osteopenia are seen in post menopausal women; this is due to the influence of estrogen on bone cells (i.e. when estrogen levels fall osteoclasts have a prolonged lifespan so more mineral is desorbed than absorbed into the bone). Peak BMD is reached around the age of 30; as we age it steadily decreases. Osteopenia is a multifactorial disorder. Risk factors include: a personal or family history, low body weight, a sedentary lifestyle, diet, smoking and other medical conditions.
Individuals with risk factors should consider screening for osteopenia/osteoporosis. The National Osteoporosis Foundation (5) lists the following as recommendations for undergoing DXA testing:
If a patient gets shorter with age, the doctor will probably order a bone mineral density
test. Other reasons your doctor may give you a BMD test:
Because there are no obvious symptoms of osteopenia, assessing how many people have this condition is difficult as many cases may go undiagnosed. A study in 2007 stated that approximately 33.6 million adult Americans were osteopenic in 2002; it went on to estimate that this figure may rise to 47.5 million by 2020. (Note that some people think osteopenia should not be treated at all.)
Appropriate treatment of osteopenia might prevent osteoporosis.
Drugs that stop bone re-absorption and hormone replacement therapy have been proven to help for osteoporosis but there is little long term evidence as to their efficacy in osteopenia. The National Osteoporosis Foundation guidelines for post-menopausal women and men past age 50 recommend that people with T-scores between -1 and -2.5 should consider taking an osteoporosis medication. Whether these medications really help osteopenia patients is a matter of some dispute.
A recent development which may assist doctors and patients to decide if osteoporosis medication is necessary is a tool called "Absolute Fracture Risk Assessment" which estimates a person’s chance of breaking a bone over a period of 10 years.
Regardless of whether medication is used, other interventions should be implemented in patients with osteopenia. Ensuring that there is sufficient calcium and vitamin D in the diet, lifestyle modifications such as stopping smoking and getting regular resistance exercise will help to maintain bone mineral density.
 The suggestions for preventing osteopenia are the same as those for preventing osteoporosis: get good nutrition (including recommended amounts of calcium and vitamin D), don’t smoke, drink only in moderation, and get exercise. People who take medicines like steroids need to be particularly vigilant. Bone density screenings can catch osteopenia before it develops into osteoporosis. Whether it is necessary to treat mild osteopenia with medication is a matter of debate.
The suggestions for preventing osteopenia are the same as those for preventing osteoporosis: get good nutrition (including recommended amounts of calcium and vitamin D), don’t smoke, drink only in moderation, and get exercise. People who take medicines like steroids need to be particularly vigilant. Bone density screenings can catch osteopenia before it develops into osteoporosis. Whether it is necessary to treat mild osteopenia with medication is a matter of debate.
1. McArdle, WD, Katch, FI and Katch, VL. Exercise physiology - Energy
nutrition and human performance. 6th edition. s.l. : Lippincott Williams
& Wilkins, 2006.
2. Hormone therapy for the prevention of bone loss in menopausal women with
osteopenia. Is it a viable option? Hohenhaus, M H, McGArry, K A and Nananda,
F C. 16, 2007, Drugs, Vol. 67, pp. 2311-2321.
3. The role of physiotherpay in the prevention and treatment of osteoporosis.
Bennell, K L, Khan, K and McKay, S. 2000, Manual Therapy, Vol. 5, pp. 198-213.
4. An observational study on the adherence to treatment guidelines of osteopenia.
Buencamino, M C A, et al. 6, 2009, Journal of womens health, Vol. 18, pp.
873-881.
5. National Osteoporosis Foundation.
http://www.nof.org.
6. Prevelence of low femoral bone density in older US adults from NHANES
III. Looker, AC, et al. 1997, J. bone mineral res., Vol. 12, pp. 1761-1786.
7. Primary
care use of FRAX (R): Absolute fracture risk assessment in postmenopausal
women and older men. Siris, ES, Baim, S and Nattiv, A. 1, 2010, Post
Graduate Medicine, Vol. 122, pp. 82-90.
8. Who's affraid of the big bad Wolff: 'Wolff's law' and bone functional
adaptation. Ruff, C, Holt, B and Trinkaus, E. 2006, Am. J. Physical anthropology,
Vol. 129, pp. 484-498.

