The most common test of bone density is called a dual-energy x-ray absorptiometry test, but everyone refers to it as a DEXA scan. A DEXA scan is similar to a plain X-ray except that it uses far less radiation. The risk posed by the radiation is very small. One advantage of a low radiation test is that bone density measurements can be followed over time from a series of DEXA scans on a regular basis. Comparing DEXA scan results allows your doctor to determine if osteoporosis treatment or prevention is directly improving bone density or if your disease is getting worse.
The DEXA determines the amount of mineralization or calcium content in bone. Osteopenia and osteoporosis are conditions in which the bones contain less calcium than they should. Less calcium means less mineralization, less mineralization means lower bone density, and lower bone density means weaker bones that are more prone to catastrophic fracture.
A DEXA scan is as fast and painless as taking a picture because, in many ways, that is precisely what is happening. A DEXA scan requires no advance preparation but you should notify the medical staff if you have recently had another radiological test. You will either report to the radiology department of a hospital or clinic or you may have the DEXA test at an independent radiology center. The DEXA test can be performed with a central or peripheral device. A central device is essentially a table on which you will lay while the DEXA scanning arm hovers above you (without touching you) and takes low energy X-rays of your spine or hip. A peripheral DEXA scanner is a smaller machine that is used to test the bone density in your wrist.
If you have ever had a DEXA, you will have probably heard the terms T-score or Z-score. A T-score compares your bone density to that of a young, healthy adult while a Z-score, on the other hand, compares your bone density to the bone densities of people that are your same age, weight, gender, and ethnicity. In general, the T-score is the one that you will follow. T-scores are generally reported in the negative numbers; a T-score above -1 is considered normal, a T-score between -1 and -2.5 is consistent with osteopenia, and a T-score below -2.5 indicates osteoporosis. The lower your T-score, on a negative number scale, the lower your bone density. In other words, you will want to keep or reach a T-score that is higher than -1. When T-scores are compared over time, it is best to measure the density from the same area of bone each time, ideally, with the same DEXA scanning device.
One downside is that DEXA is a two-dimensional look at a bone and yields a value in g/cm2 rather than a volumetric density (g/cm3) This results in a systematic overestimation of bone density in larger bones, and if DEXA's are calibrated for women, they miss some low density readings in male patients.
Warning about accuracy. There are anecdotal reports of widely different values in DEXA scan results. A patient might get a T-score in one DEXA machine and a different T-score in a second machine. That’s why some people recommend patients have their bone density evaluated by the same machine from year to year. That way, even if the reading is incorrect, the trend in bone density - up or down - still tells you whether your osteoporosis treatment is working.
Q. Do bone density tests measure how strong my bones are?
A. Not directly, but they provide a proxy for strength. More importantly they are easy to do. A better measure of bone strength would require close physical examination of the bone outside the body or through invasive sampling.
Q. How good is bone density testing?
A. Good enough that it is widely accepted by the medical community.
Q. Does it hurt?
A. No! You lie on an exam table and an x-ray machine scans you. No injections are made to the body for conventional DEXA scans and there is no pain.
Q. How much radiation does my body get?
A. Not enough to worry about. Less than a chest X-ray, for instance.
Q. How often should I get a bone density test?
A. Consult your doctor about your specific situation. People who take medicines like glucosteroids or aromatase inhibitors or who have certain conditions get another density every one or two years. People with risk factors for osteoporosis are also tested every one or two years, but people past age 65 without other risk factors had been getting them every 3 to 5 years. In 2011 the U.S. Preventive Services Task Force issued a recommendation for all women past age 65 to get regular screening. The Task Force did not say how often "regular" meant. As medical tests go, a DEXA is relatively inexpensive.
A study published in the New England Journal of Medicine in 2012 indicated that 65-year-old women who tested in the normal bone density range can wait 15 years before being retested, provided there is no other reason (e.g. a fracture) to trigger an earlier test.
There has also been interest in using DEXA scans to quantify body fat, by examining adipose tissue in the abdominal region. So far this has not caught on.
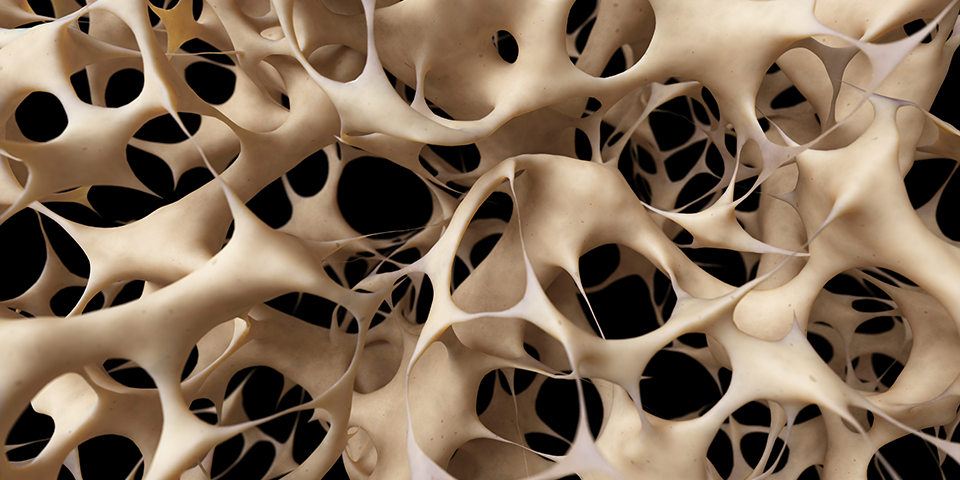
One limitation of bone density measurement by DEXA is that there are other factors that can influence the risk of fracture. Advances in radiology have given us magnetic resonance imaging, Micro-CAT, and 3-D tomography and these may end up giving us better views of bone strength in the future. The structure of the bony material at a microscopic level is important, too, and that can vary in bones of the same bulk density.
With in-vitro studies physiologists have found this architecture is an element of bone strength independent of density and that meaningful information about the architecture can be determined by CT and MRI scans. Studies in vivo have shown the micro-structure of the trabecular bone is affected more by osteoporosis treatments than bone density is. Ambitious physiologists have even used high resolution images to construct finite element models of the bone in a manner similar to engineering analyses of bridges.
Impressive as this is, it has no use for an actual patient with bone problems. Such work is useful mainly in examining the effects of new treatments in general.
It might be possible in the future, however, to use spectroscopy, diffusion, and perfusion imaging to let doctors know more about bone quality of individual patients.
A diagnostic technique called Dual X-ray laser (DXL) has been proposed as a method for estimating bone density. Tests show it is less accurate than DEXA and not widely available the way DEXA is, so it is not commonly used for osteoporosis diagnosis.
At one time a technique called radiographic absorptiometry was of interest, and it seemed to produce good results, but it never caught on, perhaps for economic reasons.
More recently, contact ultrasound bone analysis (CUBA) has been tried an in tests shows good results. It may be particularly effective in patients with arthritis.
Other techniques called spectroscopic microscopy and infrared spectroscopic imaging are said to allow measurement of small changes in bone composition.
But these require bone biopsies, so will not be used in routine screening or diagnosis.
Antiresorptive treatments typically go on for five years or more. The patient and doctor want some assurance the treatment is working, and DEXA scans provide quantitative numbers. Although not a direct measure of risk reduction, the bone density readings - when done regularly and tracked - can provide evidencr of the efficacy of antiresorptive treatment.
Recognizing there is not a direct correlation between the results of DEXA scans and the tendency to bone fractures, the medical field has started talking about "bone quality". An NIH conference defined this as "the sum total of characteristics of the bone that influence the bone's resistance to fracture." Bone quality is supposed to capture everything, but in an essay in PLoS Medicine several Finish scientists pointed out that a metric that can't be measured isn't much of a metric and concluded the term was an empty term. They suggest the term whole bone strength be preferred to bone quality.
The 25-hydroxy vitamin D test is given to bone patients to determine how much vitamin D is in the body. Blood counts (white cells, red cells, platelets) are also taken when trying to diagnose bone problems. Parathyroid hormone levels are examined to screen for hyperparathyroidism. Testosterone levels may be measured in men with low bone densities. These are all blood tests. Doctors may also order a test to measure calcium levels in the urine. Ultrasound, commonly used for imaging, can be used to estimate bone density in the heel.
CT scans can be employed to estimate bone density and are of particular use for examination of the spinal cord. It is not often used because of the cost and the large amount of radiation applied to the body can have negative effects.
A recent University of Pittsburgh study found that many methods of screening for osteoporosis were medically effective, and that none was clearly more cost effective than others.

