Research and development in orthopedic biomaterials is set to challenge the use of autografts and allografts and to establish synthetic bone as the preferred option for the nearly half-million spinal fusion procedures and other bone grafts annually performed in the United States.
Autogenous (autologous) bone has been the preferred implant for most bone graft procedures. This is bone taken from one part of the patient's skeleton and implanted in another partm and accounts for approximately 60 percent of bone grafts in the US. Allograft (bone from a cadaver) makes up 34 percent of bone implants, while other materials account for 7 percent. Autogenous grafts have some disadvantages. Harvesting bone from within the body can cause chronic pain, significant blood loss, infection and other complications, and prolonged hospital stay and recovery time.
Allograft, the second most frequent technique, precludes the need for a second surgery. Allograft also may present a risk of viral infection. In addition, the effectiveness of allograft material is inconsistent. Processing the tissue to lower contamination risk can substantially degrade the donated bone's biologic and mechanical properties. Also, a constant supply is not assured; for instance donor bone could not be always available at the time of surgery.
A variety of synthetic bone graft substitutes has become available in recent years. Synthetic bone graft substitutes should possess similar mechanical characteristics to that of the cortical bone being replaced. These characteristics include tensile strength and modulus of elasticity similar to that of bone to prevent stress shielding as well as maintaining adequate toughness to. prevent, under cyclic loading, fatigue fracture
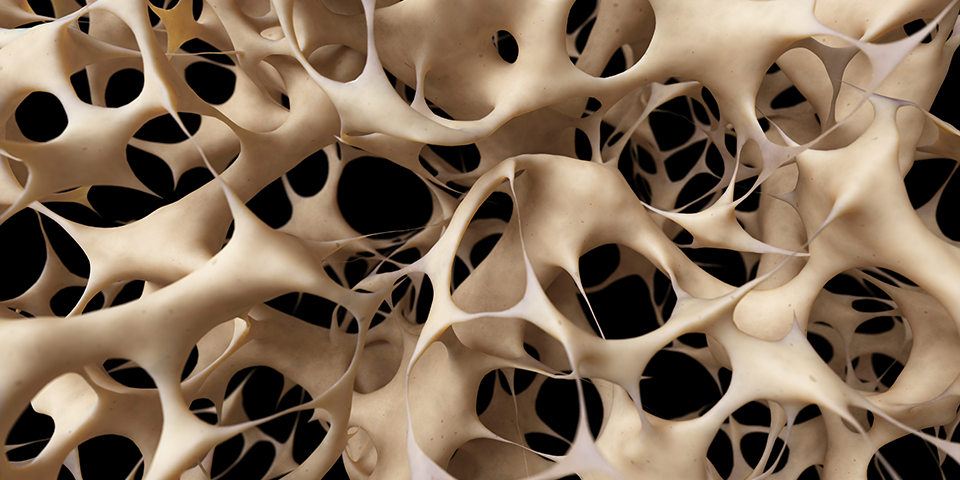
A tricalcium phosphate scaffold intended as bone void filler in trauma and spinal procedures has been approved for use in the the United States, Australia, and the European Union. The porous, fine-particle structure encourages the flow of blood and nutrients through the matrix which is gradually replaced by structured bone similar to adjacent trabecular bone. The matrix guides regeneration of host bone in three dimensions. The polyporosity of resorbable calcium phosphate allows interaction with host bone. The fine nano-particle composition enhances resorption, facilitating an effective and rapid bone remodeling.
The use of silicate-substituted calcium phosphate (Si-CaP) is focused especially for orthopedic applications (i.e. filler for gaps and voids that are not directly correlated to the stability of the bony structure).
These products provide a bone void filler that will be resorbed and replaced by bone during the healing process. Studies have shown that an optimal amount of silicate enhances local bone bioactivity; and this is supported by the finding that a crystalline silicate-substituted porous calcium phosphate containing 0.4-1.6% substituted as silicate showed higher in vivo bioactivity than silicate-free materials.
More on the materials used for bone implants.
Wolverine - the X-Man mutant - has metal bones. His skeletal structure is made of the fantasy metal Adamatium. If science fiction presagees the real world, could we someday have replacement bones like Wolverine - super strong metal? For the foreseeable future, the answer is "no". First, metal may be suited to a detached exoskeleton (e.g. a knight's armor, a car.) But alleys metallurgists and biomedical engineers know about are ill-suited to use as synthetic bone.
Would you want artificial bones? It's possible to imagine a future where synthetic bones are superior to natural ones. In such a world, athletes would be tempted to replace healthy natural bone with artificial ones. Although plausible, this doesn't appear to be on the horizon.

